Anatomy of the Cardiovascular System
- Consists of the heart, blood vessels and blood.
The Heart
Four chambered structure composed mainly of cardiac tissue. Right side of the heart moves deoxygenated blood to the lungs (pulmonary circulation), while the left side moves oxygenated blood to the rest of the body (systematic Circulation).
- Atria: Thin walled structures where blood is received from the venae Cavae or the pulmonary arteries. Contract to push blood into ventricles
- Ventricle: Much more muscular since more powerful contractions are needed.
- Atrioventricular Valves separate the atria and ventricles while the semilunar valves separate the ventricles from the vasculature (arteries, veins and capillaries).
- Tricuspid Valve is the valve between the right atria and ventricle
- Bicuspid (mitral) Valve is the valve between the left atria and ventricle
- Pulmonary Valve is the valve that separates the left ventricle from the aorta
- Aortic Valve is the valve that separates the left ventricle from the aorta.
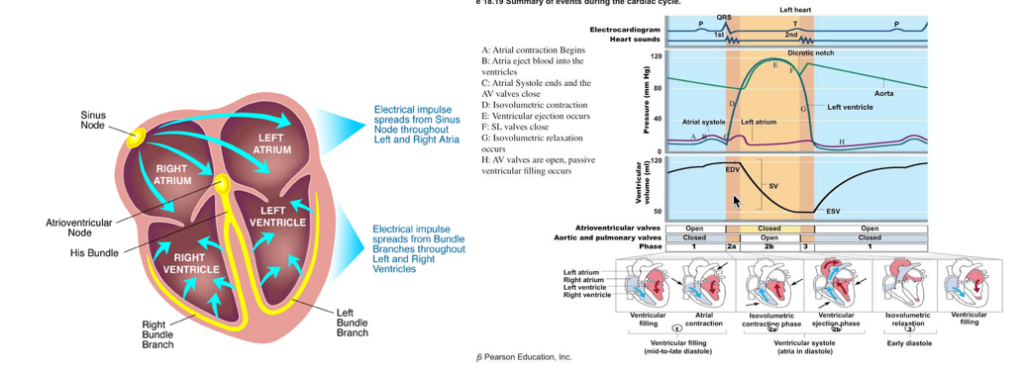
Electric Conduction of the Heart
- Impulse initiation occurs at the SA node. Node generates 60-100 signals per minute without neurological input. Located in the wall of the right atrium.
- Causes a depolarization wave which causes the two atria to contract simultaneously.
- Most ventricular filling is passive, but atrial systole (contraction) results in an increase in atrial pressure that forces a little more blood into the ventricles
- Called the atrial kick, can add 5-30% of cardiac output
- Signal then reaches the AV node which is located at the junction between the atria and the ventricles.
- Signal is delayed to allow ventricles to fill completely.
- Signal then travels down the bundles of His and its branches. This is located in the interventricular septum (wall).
- Signal then goes to the Purkinje fibers which subsequently distribute electric impulse throughout the ventricular muscles.
- Intercalated Discs connect the muscle cells. These discs contain many gap junctions which directly connect the cytoplasm of adjacent cells. This allows for a coordinated ventricular contraction.
- Normal heart beat is between 60-100 beats per minute and this can occur without any neurological input. Sympathetic would speed up the heart while parasympathetic would slow down the heart through the vagus nerve.
Contraction
- Systole: Ventricular contraction and AV valves closed. Blood is pumped out of ventricles
- Diastole: Heart is relaxed and semilunar valves are open. Blood from atria fills the ventricles.
- Elasticity of large arteries allows vessels to maintain sufficient pressure while the heart is relaxed.
- Cardiac Output: is the total blood volume pumped by a ventricle in a minute.
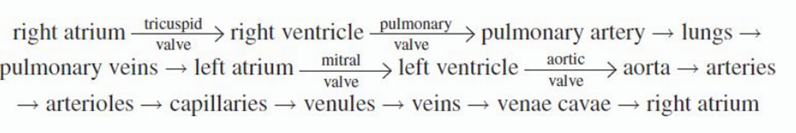
The Vasculature
- Blood travels away from the heart in arteries, the largest artery is the aorta. Major arteries like the coronary, common carotid, subclavian, and renal arteries divide the bloodflow from the aorta to different parts of the body.
- Arteries branch into arterioles which leads to capillaries.
- Venules are formed when capillaries join together on the venous side. These join to form veins.
- Venous blood empties into the inferior and superior vena cave which enter into the right side of the heart.
- All vessels are lined by endothelial cells which help to maintain the vessel by releasing chemicals that aid in vasodilation and constriction.
- Also allow for white blood cells to pass through the vessel wall and the tissue
- Cells also release chemicals that are necessary for blood clotting when the cells become damaged.
- Arteries have much more smooth muscle than veins.
Arteries
- Only arteries that do not contain oxygenated blood are the pulmonary artery and the umbilical artery.
- Are highly muscular and elastic in order to create a resistance to the flow of blood.
- Left heart must generate high pressures, then the elastic recoil of the artery walls maintains a high pressure to force the blood forward.
Capillaries
- Vessels with a single endothelial cell layer. RBC’s must pass through in a single file line.
- Thin walls allow for easy diffusion of gases, nutrients and wastes.
- Are quite delicate. If damaged, can cause blood to leak into interstitial space. Usually results in a bruise
Veins
- Thin walled, inelastic vessels that transport blood to the heart. And all carry deoxygenated blood except the pulmonary and umbilical.
- Venules are smaller venous structures that connect capilliaries.
- There is less recoil than arteries due to the smaller amount of smooth muscle. This allows the veins to stretch.
- There is always more blood (3/4th) in the venous circulation
- Downward pressure of gravity needs to be counteracted. Larger veins use valves.
- Additionally, skeletal muscles squeeze the veins to make up for their lack of smooth muscle. This propels the blood towards the heart.
Circulation
- A portal system is where blood will pass through two capillary beds instead of the standard one.
- Hepatic Portal: blood leaving the capillary beds in the walls of the gut pass through the hepatic portal vein before reaching the capillary beds in the liver
- Hypophyseal portal: blood leaving capillary bed in hypothalamus travel to capillary bed in the anterior pituitary
- Renal Portal: blood leaving the glomerulus travels through an efferent arteriole before surrounding a nephron in a capillary network called the vasa recta.
Blood
Composition
- Is about 55% liquid and 45% cells.
- Plasma is the liquid portion of blood and it is an aqueous mixture of nutrients, salts, respiratory gases, hormones and blood proteins.
- Serum is plasma with the clotting factors removed.
- All cells can be divided into: erythrocytes, leukocytes and platelets
Erythrocytes –Red Blood Cells
- Specialized cell designed for oxygen transport. Oxygen cannot dissolve in cytoplasm since it is nonpolar and therefore has low solubility in aqueous environments.
- Uses hemoglobin to bind four molecules of oxygen. Each RBC can carry ~ 1 Billion molecules of oxygen.
- Are biconcave which increases surface area and helps in travel through capillaries.
- Mature RBCs do not have a nucleus, mitochondria, and other membrane bound organelles.
- Makes space for hemoglobin. Loss of mitochondria also ensures that oxygen is not used before reaching peripheral tissue.
- Rely entirely on glycolysis for ATP. Lactic acid is the main byproduct of this type of metabolism.
- Since no nucleus present. Only have a life span of 120 days and then must be recycled since they cannot divide.
- Hemoglobin [grams per deciliter] and Hematocrit [%] can measure the quantity of RBCs in the blood
- Hematocrit is a measure of how much the blood is RBCs.
- Normal range is 13.5-17.5 & 41-53% for males and 12-16 & 36-46% for females
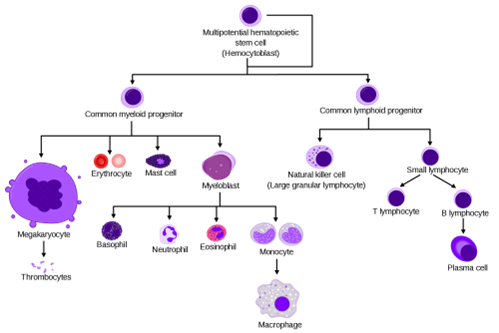
Leukocytes – White Blood Cells
- Comprise less than one percent of total blood volume. But can massively increase during critical conditions such as infection.
- Granulocytes: contain cytoplasmic granules that are visible by microscopy. The granules contain compounds that are toxic to invading microbes, and these contents can be released through exocytosis.
- These are involved in inflammatory reactions, allergies, pus formation, and destruction of bacteria + parasites.
- Consist of neutrophils, eosinophils, and basophils
- Agranulocytes: Do not contain granules that are released by exocytosis. These consist of lymphocytes & monocytes.
- Lymphocytes: More involved in specific immune response.
- Can also act as primary responders against infection. Or as long-term memory banks for pathogen recognition.
- Vaccines work by training these cells.
- Maturation can take place in one of three locations. Those formed in bone marrow are termed B-cells (antibody generation), those formed in thymus are termed T-cells (kill infected cells)
- Monocytes: phagocytize foreign matter such as bacteria.
- Once they leave the bloodstream and enter an organ, these are termed Macrophages.
- Each organ has a different name as well: in nervous system – microglia, in skin – Langerhans Cells, in bone –Osteoclasts.
- Lymphocytes: More involved in specific immune response.
Thrombocytes – Platelets
- Cell fragments or shards that are released from cells in bone marrow called megakaryocytes.
- Assist in blood clotting and are present in high concentrations.
Production of blood cells and platelets is called hematopoiesis. Erythropoietin (secreted by kidneys) stimulates RBC development. Thrombopoietin (secreted by liver and kidney) stimulates platelet development.
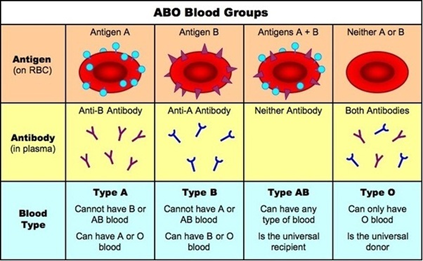
Blood Antigens
An antigen is a specific target to which the immune system can react.
- Antigens are stimuli for B-cells to make antibodies that specifically target that antigen. As such, antibodies cannot be found for antigens which the body has not been exposed to.
ABO antigens
- System is composed of three alleles for blood type. A & B alleles are co-dominant. O allele is recessive.
- Have the antigens due to E. coliin the gut.
RH Factor
- Rh positive refers to the presence of a specific allele called D. One positive allele will be enough for the protein to be expressed.
- Is of main concern for maternal-fetal medicine since Rh antibodies can cross the placenta and cause erythroblastosis fetalis.
- This condition is when a Rh- mother is exposed to the Rh+ blood of the first baby and starts producing anti-Rh antibodies. These antibodies will cross over the placenta and harm the second baby if it is also Rh+.
Physiology of the Cardiovascular System
Blood Pressure
- Measured with a sphygmomanometer and is an indication of how effective the circulatory system is functioning.
- Pressure gradually drops from the arterial to venous circulation and the largest drop occurs across the arterioles.
- Analogy with an electric circuit where the blood pressure is the driving force as compared to voltage:
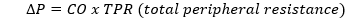
- The longer a blood vessel the more resistance it offers and the larger a cross section, the less resistance it offers.
- Opening capillary beds will result in a decreased vascular resistance and thus an increased cardiac output.
- Regulated by baroreceptors in the walls of the vasculature. These detect changes in the mechanical forces.
- When BP too low, sympathetic nervous system is stimulated, which then causes vasoconstriction, and thus increases blood pressure.
- If osmolarity is too high, ADH is released which increases blood volume and thus increases BP.
- Aldosterone increases salt retention at kidneys and therefore increases blood volume and pressure
- If BP gets too high, heart rate slows and vasculature relaxes. ANP is also secreted in the atrial cells to promote salt excretion and thus lower BP.
Gas and Solute Exchange
- At capillaries, Oxygen and nutrients diffuse out of the blood and into tissues while waste products like carbon dioxide, urea, hydrogen ions diffuse into the blood.
- Hormones are also secreted into capillaries and travel with the circulation.
- This all works on concentration gradients. One side of the capillary will always have a higher concentration of a given substance than the other.
Oxygen
- Carried by hemoglobin in the blood. Heme binds to the oxygen molecule. Oxygen molecule bonds to the groups central iron atom through a redox reaction.
- Some is also diffused into the blood plasma but this amount is negligible.
- Can be measured using partial pressure of O2 (PaO2) which has a normal range of 70-100 mmHg. Or by using Oxygen Saturation, the percentage of hemoglobin molecules carrying oxygen (normal range is above 97%).
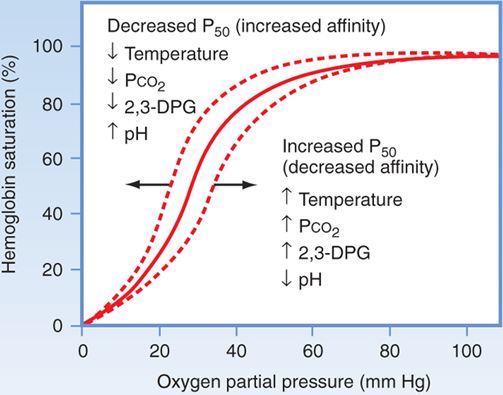
- In the lungs, oxygen diffuses into the alveolar capillaries. Once one oxygen binds to a heme group, the shape of hemoglobin relaxes and thus increases its affinity to oxygen.
- Called cooperative bonding and has an S-shaped dissociation curve. The more oxygen it binds to, the easier it is to bind more oxygen. More Oxygen that leaves, makes it easier for additional oxygen to leave.
Carbon Dioxide
- Only a small percentage of CO2 is carried in the blood to the lungs. It can also be carried by hemoglobin, but in much less capacity as compared to oxygen.
- Most of the carbon dioxide exits blood as the bicarbonate ion:
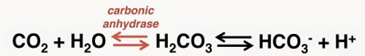
- If carbon dioxide production is increased, then pH will decrease. Influx of Hydrogen ions can bond to hemoglobin which ultimately decreases the hemoglobin’s affinity to oxygen. This is known as the Bohr Effect.
- Fetal hemoglobin has a higher affinity for oxygen than adult hemoglobin. Which means that the curve is shifted to the left for fetuses.
Nutrients, Wastes and Hormones
- Carbs and amino acids are absorbed into the capillaries of the small intestine and enter systematic circulation via the hepatic portal system.
- Fats are absorbed into lacteals in the small intestine, bypass hepatic portal system
- Fats are packaged as lipoproteins which become water soluble.
- Wastes travel down concentration gradient from tissues to capillaries. Are then filtered out at the kidneys
- Hormones enter the circulation in or near the organ they are produced at.
- Usually occurs by exocytosis, some can bind to proteins.
Fluid Balance
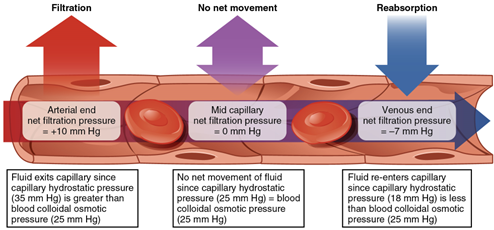
- Hydrostatic Pressure: force per unit area that the blood exerts against the vessel walls. Generated by the contraction of the heart and the elasticity of the arteries.
- Measured upstream of the large arteries as blood pressure
- Pushes fluids out of the bloodstream and into interstitium
- Osmotic Pressure: sucking pressure generated by solutes as they attempt to draw water into the bloodstream.
- Oncotic Pressure: another name for above since it can be mainly attribute to the bloods plasma proteins.
- At arteriole end of capillary bed, the hydrostatic pressure is much larger than the oncotic pressure, and there is a net efflux of water out of the capillary.
- Hydrostatic pressure drops significantly as water moves out, and osmotic pressure stays the same. So at the venule end, there is a net influx of water back into circulation.
- Balancing of opposing pressures is called Starling Forces.
- Edema is the accumulation of excess fluid in the interstitium
- Some interstitial fluid is taken up the lymphatic system. Most lymph returns to the circulatory system through the thoracic duct.
Coagulation
- Clots are composed of coagulating factors (proteins) and platelets. These are meant to prevent blood loss
- If endothelium is damaged, the underlying connective tissue is exposed. This tissue contains collagen and tissue factor
- When platelets come into contact with collagen, they sense that there is an injury.
- They then begin to aggregate (clump) together
- At the same time, coagulation factors sense the tissue factor and initiate a complex activation cascade.
- Endpoint of cascade is the activation of prothrombin which forms thrombin by thromboplastin.
- Thrombin then converts fibrinogen to fibrin.
- Fibrin forms small fibers that aggregate and cross-link into woven structures (like a net). This forms a stable clot over the area that is damaged.
- Blood clotting or thrombus formation occur when a blood vessel is injured. Together the cells and protein form a network of cells that is dense enough to plug the injury and prevent blood loss so that the wound can be repaired.
- Involves activation of integrin molecules when the platelets come into contact with the exposed connective tissue.
- Clot is broken down by plasmin which comes from plasminogen.
